What to Expect During Diabetic Foot Ulcer Treatment: A Patient’s Guide
If you’ve been diagnosed with a diabetic foot ulcer, understanding what to expect during diabetic foot ulcer treatment can help reduce anxiety and improve your outcomes. The treatment process is comprehensive and requires patience, but with proper medical care and your active participation, most diabetic foot ulcers can heal successfully.
Understanding Your Initial Evaluation
Comprehensive Assessment
Your diabetic foot ulcer treatment begins with a thorough evaluation that typically includes:
Medical History Review: Your healthcare provider will examine your diabetes management history, previous ulcers, current medications, and overall health status. This information helps determine the best treatment approach for your specific situation.
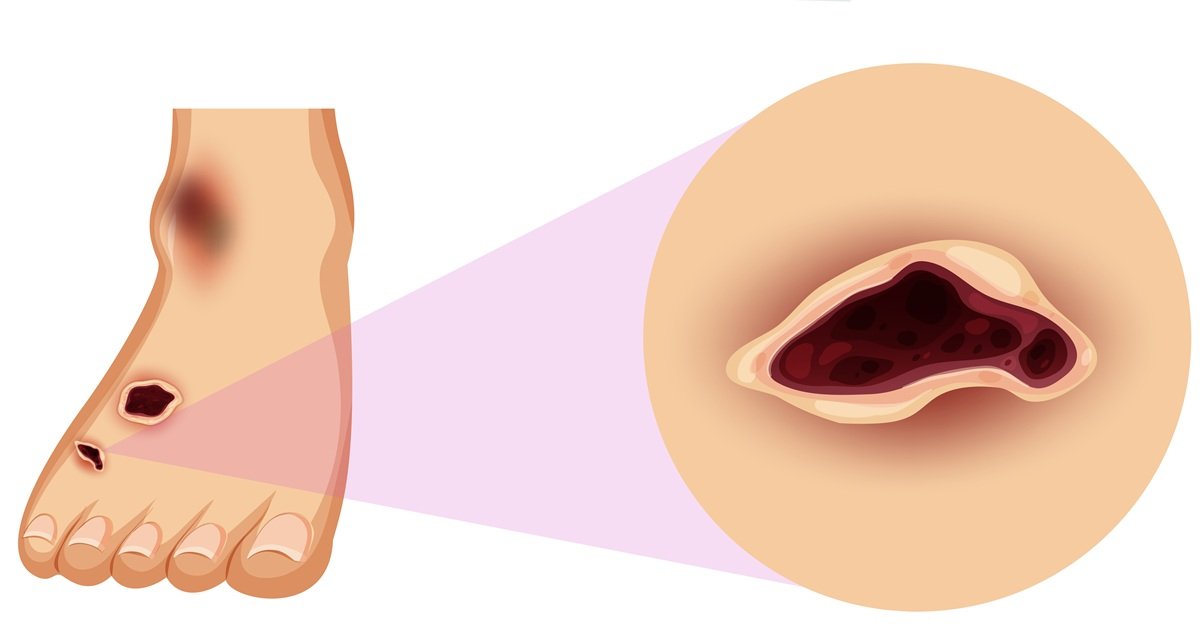
Physical Examination: The ulcer will be carefully measured, photographed, and assessed for depth, signs of infection, and surrounding tissue health. Your doctor will also check your foot’s circulation, nerve function, and overall structure.
Diagnostic Tests: Depending on your ulcer’s severity, you may need X-rays to check for bone involvement, blood tests to assess infection markers and blood sugar control, or specialized circulation studies.
Wound Grading: Your ulcer will be classified using standardized grading systems to determine severity and guide treatment decisions. This classification helps predict healing time and potential complications.
The Treatment Process: What Happens Next
Stage 1: Infection Control and Debridement
Immediate Priorities: If infection is present, controlling it becomes the top priority in your diabetic foot ulcer treatment. This may involve:
- Antibiotic therapy either oral or intravenous, depending on infection severity
- Surgical debridement to remove dead, damaged, or infected tissue
- Daily wound cleaning with appropriate solutions
- Culture testing to identify specific bacteria and guide antibiotic selection
Debridement Process: This crucial step removes barriers to healing. While it may sound concerning, debridement is typically not painful when performed on dead tissue. Your healthcare provider will explain the process and ensure your comfort throughout.
Stage 2: Creating Optimal Healing Conditions
Wound Bed Preparation: Once infection is controlled, your treatment focuses on creating the best environment for healing:
- Moisture balance using specialized dressings that keep the wound appropriately moist
- Advanced wound dressings that may include antimicrobial agents, growth factors, or bioengineered materials
- Pressure redistribution through special shoes, boots, or custom orthotics
- Offloading devices to remove pressure from the ulcer site
Blood Sugar Management: Optimal glucose control is essential for healing. Your treatment team may adjust your diabetes medications or recommend dietary changes to maintain stable blood sugar levels throughout the healing process.
Stage 3: Promoting Active Healing
Advanced Therapies: Depending on your ulcer’s characteristics and healing progress, your diabetic foot ulcer treatment may include:
- Bioengineered skin substitutes that provide growth factors and scaffolding for new tissue
- Negative pressure wound therapy using controlled suction to promote blood flow and remove excess fluid
- Hyperbaric oxygen therapy to increase oxygen delivery to the wound
- Growth factor applications to stimulate cellular repair processes
Regular Monitoring: Healing progress is tracked through regular measurements, photographs, and assessments. This monitoring helps your healthcare provider adjust treatments as needed.
Timeline Expectations for Healing
Realistic Healing Timeframes
Understanding the Process: Diabetic foot ulcer healing is typically slower than normal wound healing. Several factors influence your timeline:
Mild to Moderate Ulcers: May heal within 6-12 weeks with proper treatment and good diabetes control.
Severe or Deep Ulcers: Can take 3-6 months or longer, especially if bone involvement or significant infection was present initially.
Factors Affecting Healing Time:
- Blood sugar control quality
- Circulation to the affected area
- Infection presence and severity
- Ulcer size and depth
- Patient compliance with treatment
- Overall health status
- Smoking status
Stages of Healing You’ll Notice
Week 1-2: Focus on infection control and establishing clean wound bed Week 3-6: Granulation tissue development (healthy red tissue growth) Week 6-12: Wound contraction and epithelialization (skin growing over the wound) Beyond 12 weeks: Continued healing and tissue strengthening
Your Role in Treatment Success
Daily Wound Care Responsibilities
Home Care Tasks: Your active participation is crucial for successful diabetic foot ulcer treatment:
- Dressing changes as instructed by your healthcare provider
- Daily wound inspection for signs of improvement or problems
- Medication compliance including antibiotics and diabetes medications
- Activity modification to avoid pressure on the healing ulcer
- Blood sugar monitoring to maintain optimal glucose control
Lifestyle Modifications
Supporting Healing: Several lifestyle factors significantly impact your treatment success:
Nutrition: Adequate protein, vitamins, and minerals support tissue repair. Your healthcare provider may recommend specific dietary changes or supplements.
Smoking Cessation: If you smoke, quitting dramatically improves circulation and healing potential.
Activity Management: Balancing appropriate activity with wound protection is essential. Your healthcare team will provide specific guidelines.
Stress Management: Chronic stress can impair healing, so incorporating stress-reduction techniques may benefit your recovery.
Warning Signs to Watch For
When to Contact Your Healthcare Provider Immediately
During diabetic foot ulcer treatment, certain signs require urgent attention:
Infection Indicators:
- Increased redness spreading beyond the wound area
- Swelling that worsens or doesn’t improve
- Increased warmth around the wound
- Pus or foul-smelling drainage
- Red streaking extending from the wound
- Fever or chills
- Increased pain
Healing Concerns:
- Wound appears larger or deeper
- New areas of skin breakdown
- Persistent bleeding
- Signs that the wound is not progressing as expected
Treatment Adjustments and Monitoring
How Treatment Evolves
Adaptive Approach: Your diabetic foot ulcer treatment plan will likely evolve as healing progresses:
Weekly Assessments: Regular visits allow for treatment modifications based on healing progress. Dressing types may change, medications may be adjusted, and new therapies may be introduced.
Problem-Solving: If healing plateaus or complications arise, your healthcare provider may recommend additional specialists, advanced treatments, or diagnostic tests.
Success Indicators: Your treatment team tracks multiple factors including wound size reduction, healthy tissue growth, absence of infection, and improved circulation.
Preventing Future Ulcers
Long-Term Management
Post-Healing Care: Even after successful treatment, preventing recurrence is crucial:
- Continued foot monitoring for early problem detection
- Proper footwear to prevent pressure points
- Regular podiatric care for nail trimming and callus management
- Ongoing diabetes management to maintain optimal blood sugar control
- Patient education about foot care and risk factors
Working with Your Healthcare Team
Collaborative Care Approach
Team Members: Successful diabetic foot ulcer treatment often involves multiple specialists:
- Primary care physician for overall diabetes management
- Wound care specialist for advanced treatment options
- Podiatrist for foot-specific care
- Endocrinologist for complex diabetes management
- Nutritionist for dietary optimization
- Certified diabetes educator for ongoing education and support
Communication Expectations
Staying Informed: Your healthcare team should:
- Explain each treatment step clearly
- Provide written home care instructions
- Establish clear communication channels for questions
- Schedule appropriate follow-up visits
- Coordinate care between specialists
Comprehensive Approach to Diabetic Foot Ulcer Cure
A modern holistic approach to diabetic foot ulcer treatment includes:
Evidence-Based Care: Using the latest research and treatment protocols to optimize healing outcomes for each patient.
Patient Education: Ensuring you understand every aspect of your treatment and how to participate actively in your healing.
Coordinated Care: Working closely with specialists when needed to provide comprehensive treatment.
Ongoing Support: Providing continuous monitoring and adjustment of treatment plans as your needs evolve.
Prevention Focus: Helping you develop strategies to prevent future ulcers through education and ongoing care.
Taking the Next Step
If you’re facing diabetic foot ulcer treatment, remember that early intervention and consistent care significantly improve outcomes. Don’t let concerns about the treatment process delay seeking care – the sooner treatment begins, the better your chances for complete healing.
Schedule your consultation today to begin comprehensive diabetic foot ulcer treatment. With proper medical care, your commitment to the treatment process, and patience with the healing timeline, you can achieve successful wound healing and return to your normal activities.
Remember, diabetic foot ulcer treatment is a partnership between you and your healthcare team. Your active participation, combined with professional medical expertise, creates the best foundation for healing success.
Resources
Professional Organizations
- American Podiatric Medical Association – https://www.apma.org/ – Comprehensive information on diabetic foot care and ulcer prevention strategies.
- American Diabetes Association – https://www.diabetes.org/ – Evidence-based resources for diabetes management and foot care guidelines.
- Wound Healing Society – https://www.woundheal.org/ – Scientific research and clinical guidelines for advanced wound healing treatments.
Educational Resources
- National Institute of Diabetes and Digestive and Kidney Diseases – https://www.niddk.nih.gov/ – Federal resource for diabetes complications including diabetic foot ulcers.
- Centers for Disease Control and Prevention – https://www.cdc.gov/diabetes/ – Public health information on diabetes management and complication prevention.
Clinical Publications
- Diabetes Care Journal – Latest research on diabetic complications and treatment protocols
- Wound Repair and Regeneration – Peer-reviewed journal focusing on wound healing science and clinical applications
Dr. Hina Zaman’s family medicine practice in Murphy, TX, provides comprehensive medical services for patients throughout North Texas. We’re committed to helping you achieve successful healing through evidence-based care and patient education.



